STROKE SPECIALIST IN NASHIK
- Stroke
- Stroke Case Studies
- Stroke Videos
- Stroke Testimonials
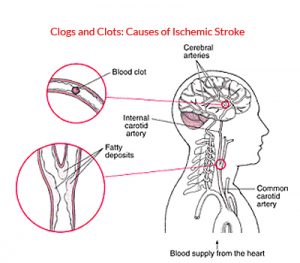
An ischemic stroke is death of an area of brain tissue (cerebral infarction) resulting from an inadequate supply of blood and oxygen to the brain due to blockage of an artery.
An ischemic stroke typically results from blockage of an artery that supplies blood to the brain. Common causes: Commonly, blockages are blood clots (thrombi) or pieces of fatty deposits (atheromas, or plaques) due to atherosclerosis. Such blockages often occur in the following ways:
- By forming in and blocking an artery: An atheroma in the wall of an artery may continue to accumulate fatty material and become large enough to block the artery.
- By traveling from another artery to an artery in the brain: A piece of an atheroma or a blood clot in the wall of an artery can break off and travel through the bloodstream (becoming an embolus). The embolus may then lodge in an artery that supplies the brain and block blood flow there.
- By traveling from the heart to the brain: Blood clots may form in the heart or on a heart valve, particularly artificial valves and valves that have been damaged by infection of the heart’s lining (endocarditis). Strokes due to such blood clots are most common among people who have recently had heart surgery, who have had a heart attack, or who have a heart valve disorder or an abnormal heart rhythm (arrhythmia), especially a fast, irregular heart rhythm called atrial fibrillation.
- Lacunar infarction In lacunar infarction, one of the small arteries deep in the brain becomes blocked when part of its wall deteriorates and is replaced by a mixture of fat and connective tissue—a disorder called lipohyalinosis. Lacunar infarction tends to occur in older people with diabetes or poorly controlled high blood pressure.The prognosis is usually good.
- Blood disorders: Some disorders, such as an excess of red blood cells (polycythemia), antiphospholipid syndrome, and a hyperhomocysteinemia, make blood more likely to clot. In children, sickle cell disease can cause ischemic stroke.
- Oral contraceptives: Taking oral contraceptives, particularly those with a high estrogen dose, increases the risk of blood clots.
 Risk factors:The major risk factors for ischemic stroke are
Risk factors:The major risk factors for ischemic stroke are
- Atherosclerosis (narrowing or blockage of arteries by patchy deposits of fatty material in the walls of arteries)
- High cholesterol levels
- High blood pressure
- Diabetes
- Smoking
Other risk factors include
- Having relatives who have had a stroke
- Consuming too much alcohol
- Using cocaine or amphetamines
- Having an abnormal heart rhythm called atrial fibrillation
- Having another heart disorder, such as a heart attack or infective endocarditis (infection of the heart’s lining)
- Having inflamed blood vessels (vasculitis) Obesity.
- Lack of excersize.
- Eating an unhealthy diet (such as one high in saturated fats, trans fats, and calories)
- Having a clotting disorder

- Blindness in one eye
- Inability to see out of the same side in both eyes
- Abnormal sensations, weakness, or paralysis in one arm or leg or on one side of the body
- Slurred speech or unable to speak.
- Dizziness and vertigo
- Imbalance
- Double vision
- Generalized weakness on both sides of the body
- Computed tomography (CT) is usually done first. CT helps distinguish an ischemic stroke from a hemorrhagic stroke, a brain tumor, an abscess, and other structural abnormalities.
- Diffusion-weighted magnetic resonance imaging (MRI), which can detect ischemic strokes within minutes of their start, may be done next.
Tests for causes may include the following:
- Electrocardiography (ECG) to look for abnormal heart rhythms
- Echocardiography to check the heart for blood clots, pumping or structural abnormalities, and valve disorders
- Imaging tests—color Doppler ultrasonography, magnetic resonance angiography, CT angiography, or cerebral (standard) angiography to determine whether arteries, especially the internal carotid arteries, are blocked or narrowed
- Blood tests to check for anemia, polycythemia, blood clotting disorders, vasculitis, and some infections (such as heart valve infections and syphilis) and for risk factors such as high cholesterol levels or diabetes
People who have any symptom suggesting an ischemic stroke should go to an emergency department immediately. The earlier the treatment, the better are the chances for recovery.Specific treatment of stroke may include drugs to break up blood clots (thrombolytic drugs) and drugs to make blood less likely to clot (antiplatelet drugs and anticoagulants), followed by rehabilitation. At some specialized centers, blood clots are physically removed from arteries (called mechanical thrombectomy).Measures to prevent another stroke include control of risk factors (including high blood pressure, diabetes, and high cholesterol levels), use of drugs that make blood less likely to clot, and sometimes surgery or angioplasty to open blocked arteries.Thrombolytic (fibrinolytic) drugs:In certain circumstances, a drug called tissue plasminogen activator (tPA) is given to patients intravenously to break up clots and help restore blood flow to the brain who present within 4.5 hours. After 4.5 hours, most of the damage to the brain cannot be reversed, and the risk of bleeding outweighs the possible benefit of using tPA.Intra-arterial thrombolysis At present intravenous therapy is not recommended beyond 4.5 hours. Intra-arterial thrombolysis can work up to 6-hours. Therefore patients coming between 3 to 6 hours can benefit by intra-arterial therapy. The window period can be further extended in cases of posterior circulation stroke. Patients with major vessel blockage such as internal carotid, middle cerebral artery and basilar artery are unlikely to respond to intravenous thrombolysis and can be treated better by intra-arterial means.
At present intravenous therapy is not recommended beyond 4.5 hours. Intra-arterial thrombolysis can work up to 6-hours. Therefore patients coming between 3 to 6 hours can benefit by intra-arterial therapy. The window period can be further extended in cases of posterior circulation stroke. Patients with major vessel blockage such as internal carotid, middle cerebral artery and basilar artery are unlikely to respond to intravenous thrombolysis and can be treated better by intra-arterial means.
Mechanical thrombectomy:  For this procedure, doctors use a device to physically remove the blood clot. This procedure is often done when people have had a severe stroke with large artery occlusion and have been ineffectively treated with tPA, given intravenously or by catheter. This procedure must be done within 6 to 8 hours of when symptoms began.. Mechanical thrombectomy may be useful for people who cannot be given tPA.Antiplatelet drugs and anticoagulants:If a thrombolytic drug cannot be used, most people are given aspirin as soon as they get to the hospital. If symptoms seem to be worsening, anticoagulants such as heparin are occasionally used, but their effectiveness has not been
For this procedure, doctors use a device to physically remove the blood clot. This procedure is often done when people have had a severe stroke with large artery occlusion and have been ineffectively treated with tPA, given intravenously or by catheter. This procedure must be done within 6 to 8 hours of when symptoms began.. Mechanical thrombectomy may be useful for people who cannot be given tPA.Antiplatelet drugs and anticoagulants:If a thrombolytic drug cannot be used, most people are given aspirin as soon as they get to the hospital. If symptoms seem to be worsening, anticoagulants such as heparin are occasionally used, but their effectiveness has not been
Mechanical thrombectomy in acute stroke patient
65 female known diabetic, hypertensive and heart disease presented with sudden onset rt sided weakness with loss of speech since 2 hours. NIHSS 11. MRI Brain with MRA showed acute left MCA infarct with left MCA occlusion. Post mechanical thrombectomy pt made complete recovery.






