ARTERIOVENOUS MALFORMATION
- Intracranial Atherosclerosis
- Case Studies
- Videos
- Testimonials
 Normally, arteries carry blood containing oxygen from the heart to the brain, and veins carry blood with less oxygen away from the brain and back to the heart. When an arteriovenous malformation (AVM) occurs, a tangle of blood vessels in the brain or on its surface bypasses normal brain tissue and directly diverts blood from the arteries to the veins.
Normally, arteries carry blood containing oxygen from the heart to the brain, and veins carry blood with less oxygen away from the brain and back to the heart. When an arteriovenous malformation (AVM) occurs, a tangle of blood vessels in the brain or on its surface bypasses normal brain tissue and directly diverts blood from the arteries to the veins.Brain AVMs occur in < 1 % of the general population. AVMs are more common in males than females and in younger age group. (20-40)
We do not know why AVMs occur. Brain AVMs are usually congenital, meaning someone is born with one. However, they usually are not hereditary.
Brain AVMs can occur anywhere within the brain or on the covering of the brain. This includes the four major lobes of the front part of the brain (frontal, parietal, temporal, occipital), the back part of the brain (cerebellum), the brainstem, or the ventricles (deep spaces within the brain that produce the cerebrospinal fluid).
Most AVMs do not grow or significantly change although the vessels involved may dilate.
Symptoms may vary with location
- > 50 % of patients with an AVM present with intracranial hemorrhage.
- 20% – 25% of patients with an AVM have seizures, either focal or generalized.
- 15% may have headache or hemiparesis.
A brain AVM contains abnormal blood vessels that direct blood away from normal brain tissue. These abnormal and weak blood vessels dilate over time and may eventually burst from the high pressure of blood flow from the arteries causing bleeding into the brain.
A brain AVM contains abnormal blood vessels that direct blood away from normal brain tissue. These abnormal and weak blood vessels dilate over time and may eventually burst from the high pressure of blood flow from the arteries causing bleeding into the brain.
True Arteriovenous malformation (AVM). This is the most common brain vascular malformation and consists of a tangle of abnormal vessels connecting arteries and veins with no normal intervening brain tissue.Occult or cryptic AVM or cavernous malformations. This is a vascular malformation in the brain that does not actively divert large amounts of blood. It may bleed and often produce seizures.Dural fistula. The covering of the brain is called the “dura mater.” When there is an abnormal connection between blood vessels that involve only this covering, it is called a dural fistula. Dural fistulas can occur in any part of the brain covering.
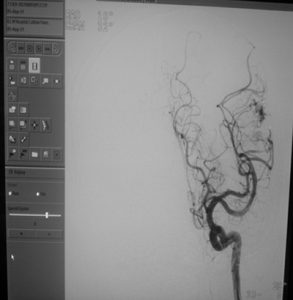
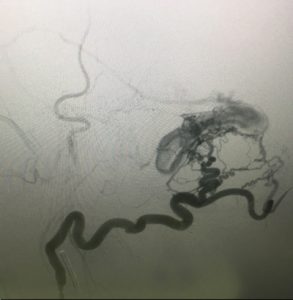
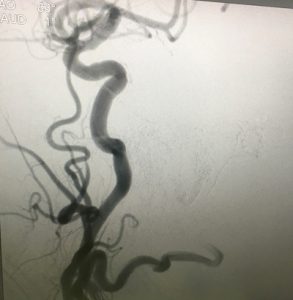
 Most AVMs are detected on either a computed tomography (CT) brain scan or with a magnetic resonance imaging (MRI) brain scan. These tests are very good at detecting brain AVMs. They also provide information about the location and size of the AVM and whether it may have bled.Cerebral angiogram – For any type of treatment involving an AVM, an angiogram may be needed to better identify the type and angioarchitecture of AVM.
Most AVMs are detected on either a computed tomography (CT) brain scan or with a magnetic resonance imaging (MRI) brain scan. These tests are very good at detecting brain AVMs. They also provide information about the location and size of the AVM and whether it may have bled.Cerebral angiogram – For any type of treatment involving an AVM, an angiogram may be needed to better identify the type and angioarchitecture of AVM.In general, an AVM may be considered for treatment if it has bled, if it is in an area of the brain that can be easily treated and if it is not too large.
This depends upon what type it is, the symptoms it may be causing and its location and size.
There are 3 modes of treatment. Endovascular embolisation, radiosurgery or surgery.These are advocated alone or in combination as per type, size and location of AVM.
- Medical Therapy. If there are no symptoms or almost none, or if an AVM is in an area of the brain that cannot be easily treated, conservative medical management may be indicated.
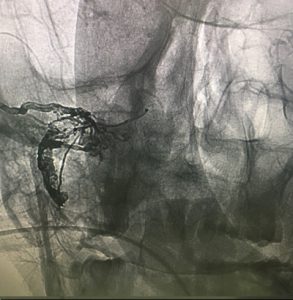
- Embolisation of AVM. It may be possible to treat part or all of the AVM by placing a catheter (small tube) inside the blood vessels that supply the AVM and blocking off the abnormal blood vessels with a variety of different materials. These include liquid tissue adhesives ONYX or glue is used to stop blood flowing to the AVM.It is frequently combined with radiosurgery or it canbe staged in multiple sessions.
- Stereotactic radiosurgery. An AVM that is not too large, but is in an area that is difficult to reach by regular surgery, may be treated by performing stereotactic radiosurgery. In this procedure a cerebral angiogram is done to localize the AVM. Focused-beam high energy sources are then concentrated on the brain AVM to produce direct damage to the vessels that will cause a scar and allow the AVM to “clot off.”
- Surgery. If an AVM has bled and/or is in an area that can be easily operated upon, then surgical removal may be recommended.
Case 1 – Young male with recurrent rt sided weakness & brain hemorrhage
21 years male patient came with headache & recurrent rt hemiparesis since 3 months. His CT brain showed a left parietal bleed. His MRA was normal. DSA showed left parietal AVM. After embolisation with onyx, there was complete recovery & the patient had no recurrent symptoms.
Case 2 – Elderly patient with brain hemorrhage & convulsions
60 years male pt presented with severe headache, convulsions & an unconscious state. MRI Brain & MRA showed rt parieto occipital bleed due to rt parieto occipital dural AV fistula. DSA confirmed the same. Post embolisation with onyx the fistula was totally obliterated & the patient made a complete recovery.