CAROTID ARTERY STENOSIS
- Carotid Artery Stenosis
- Case Studies
- Videos
- Testimonials
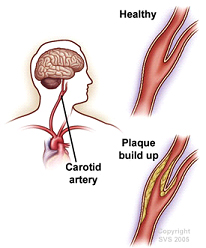 Carotid artery stenosis, occurs when the carotid arteries, the main blood vessels that carry oxygenated blood to the brain, become narrowed. The narrowing of the carotid arteries is most commonly related to atherosclerosis (a build-up of plaque, which is a deposit of fatty substances, cholesterol, cellular waste products, calcium, and fibrin in the inner lining of an artery).
Carotid artery stenosis, occurs when the carotid arteries, the main blood vessels that carry oxygenated blood to the brain, become narrowed. The narrowing of the carotid arteries is most commonly related to atherosclerosis (a build-up of plaque, which is a deposit of fatty substances, cholesterol, cellular waste products, calcium, and fibrin in the inner lining of an artery).
If the narrowing of the carotid arteries becomes severe enough to block blood flow, or a piece of atherosclerotic plaque breaks off and obstructs blood flow to the brain, a stroke may occur.
Atherosclerosis is the most common cause of carotid artery disease.Risk factors associated with atherosclerosis include:
- Older age
- Male
- Family history
- Race or ethnicity
- Genetic factors
- Hyperlipidemia (elevated fats in the blood)
- Hypertension (high blood pressure)
- Smoking
- Diabetes
- Obesity
- Diet high in saturated fat
- Lack of exercise
- Sudden weakness or clumsiness of an arm and/or leg on one side of the body
- Loss of coordination or movement
- Numbness or loss of sensation (feeling) in the face
- Numbness or loss of sensation in an arm and/or leg
- Temporary loss of vision or blurred vision
- Inability to speak clearly or slurred speech
Stroke is another indicator of carotid artery disease.
- Carotid artery doppler– a type of vascular noninvasive ultrasound study performed to assess the blood flow of the carotid arteries.
- Magnetic resonance imaging (MRI) – a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body.
- Magnetic resonance angiography (MRA)/ CTA – a noninvasive diagnostic procedure that uses a combination of magnetic resonance technology (MRI) or xrays and intravenous (IV) contrast dye to visualize blood vessels.
- Cerebral Angiography (DSA) –gold standard an invasive procedure used to assess the degree of blockage or narrowing of the carotid arteries by taking x-ray images while a contrast dye in injected. The contrast dye helps to visualize the shape and flow of blood through the arteries as x-ray images are made.
- Carotid artery disease (asymptomatic or symptomatic) in which the narrowing of the carotid artery is less than 50 percent is most often treated medically. Asymptomatic disease with less than 70 percent narrowing may also be treated medically, depending on the individual situation.Medical treatment for carotid artery disease may include:
- Modification of risk factors. Risk factors that may be modified include smoking, elevated cholesterol levels, elevated blood glucose levels, lack of exercise, poor dietary habits, and elevated blood pressure.
- Medications
- Antiplatelet medications –
- Antihyperlipidemics – medications used to lower lipids (fats) in the blood, particularly cholesterol.
- Antihypertensives – medications used to lower blood pressure.
- Antidiabetics – medications used to lower blood sugar.
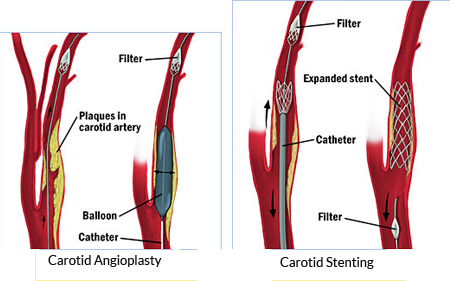 Carotid endarterectomy (CEA) is a procedure used to remove plaque and clots from the carotid arteries, located in the neckCarotid artery angioplasty with stenting (CAS). This is a minimally invasive procedure in which a very small hollow tube, or catheter, is advanced from a blood vessel in the groin to the carotid arteries. Once the catheter is in place, a balloon may be inflated to open the artery and a stent is placed.. Because there is a risk of stroke from bits of plaque breaking off during the procedure, an apparatus, called an embolic protection device, may be used.Advantages of CAS over CEA
Carotid endarterectomy (CEA) is a procedure used to remove plaque and clots from the carotid arteries, located in the neckCarotid artery angioplasty with stenting (CAS). This is a minimally invasive procedure in which a very small hollow tube, or catheter, is advanced from a blood vessel in the groin to the carotid arteries. Once the catheter is in place, a balloon may be inflated to open the artery and a stent is placed.. Because there is a risk of stroke from bits of plaque breaking off during the procedure, an apparatus, called an embolic protection device, may be used.Advantages of CAS over CEA
CAROTID STENTING
1) Carotid stenting for pt with acute vision loss & TIA’S
55/M HTN DM IHD- Post PTCA status presented with H/O acute onset left mono occular blindness and recurrent rt sided weakness. MR angiography showed lt ICA total occlusion. Post carotid stenting there was no recurrent strokes.
2) Carotid stenting for pt posted for Bypass surgery of heart.
- 50 year old male pt , hypertensive & diabetic with old h/o left hemiparesis 20 years ago had ischemic heart disease & was posted for bypass surgery
- Doppler carotid showed – left carotid 60- 70% stenosis.
Angiography showed severe stenosis > 90 % of left carotid origin. Post carotid stenting pt was asymptomatic & bypass surgery was carried out later. There were no paralysis episode during bypass surgery due to successful carotid stenting
3) Vertebral stenting for recurrent TIA’S
58 year old gentleman hypertensive & diabetic presented with recurrent giddiness imbalance & visual blurring. His MRI brain showed multiple infarcts in posterior circulation. Cerebral angiography showed severe stenosis of rt vertebral artery at its origin for which stenting was done. Post stenting there are no recurrence of his symptoms







